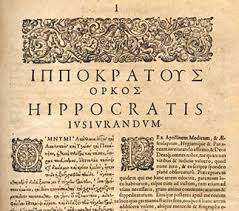
The Hippocratic Oath is an ethical code attributed to the ancient Greek physician Hippocrates, adopted as a guide to conduct by the medical profession throughout the ages and still used in the graduation ceremonies of many medical schools.
The Editors of Encyclopædia Britannica Last Updated 11-9-2014
 The part of the oath that people still quote is:
The part of the oath that people still quote is:
“With regard to healing the sick, I will devise and order for them the best diet, according to my judgment and means; and I will take care that they suffer no hurt or damage.”
It has been turned into a simple line “FIRST DO NO HARM”.
Breaking the Oath
Our belief is that Dr’s do their best to keep us well, make us well, or treat our ills. But even if they can’t, they will not do anything that could cause us harm.
We trust they will do “everything within their knowledge and skills” to follow these rules.
We have seen what happens when they don’t. Read A Catastrophic Event
What if they have the knowledge, they have the information, they have the people trained to deal with an illness, to ensure they “do no harm”, but they fail in the very basics of actually utilising the knowledge and skills at their disposal, and they do harm?
In an previous post I talked about the fact Wellington’s Capital & Coast District Health Board (CCDHB), failed us by not “bridging” Derek with Clexane when the stopped his warfarin for surgery. While investigating what happened we found out thay actually had documents that had a plan written down for people with Thrombocytopenia (low Platelet count) and a blood clotting disorder.
This plan required that if they ever stopped his warfarin, he should be put on Clexane, to prevent clotting. Unfortunately we didn’t know this.
Why didn’t we know? Because our knowledge was based on previous behaviours by CCDHB.
CCDHB Did Harm Twice
CCDHB’s Guidelines for Therapeutic Anticoagulation Management (TAM) states that Warfarin needs to be stopped for 5 days for invasive procedures. During this time you must be bridged with Clexane. Once the invasive procedure is completed, as long as you are not bleeding, you are then started back on Warfarin. You are kept on Clexane from stopping warfarin, to the point at which your INR is at a therapeutic level for you.
They don’t specifically mention a prostate biopsy in their TAM document, but they do mention procedures such as gastroscopy’s, endoscopies etc. The idea being that if it is “invasive”, i.e. taking a biopsy, where there is a risk of bleeding, Stop Warfarin, Bridge with Clexane, Restart Warfarin, stop Clexane.
We have now discovered that when Derek had his Biopsy in May 2012 CCDHB did not follow their own written procedures. They stopped Derek’s Warfarin. There was no Bridging Plan.
CCDHB’s Plan for Biopsy:
Stop Warfarin for 5 days before biopsy.
Have Biopsy.
2-3 Days after Biopsy, restart Warfarin, if bleeding has stopped.
Nowhere in the medical notes, is there any reference to Clexane. Hence we were not surprised when Derek was told to again stop warfarin for surgery.
But Wait…. There’s More.
An important piece of information we have recently found out about Warfarin.
We always believed that the ONLY time Derek was put on Warfarin and Clexane at the same time was when he first suffered his DVT and it was to try and speed up the dissolving of the DVT. WRONG!
The reason you use clexane when starting on warfarin is because, when you first start warfarin, it actually works in reverse. Until you are therapeutic, the warfarin increases coagulation of your blood, until your body adjusts, which takes around 3 days but should always be checked with INR testing. So, to prevent something going wrong i.e. a thrombotic storm, you are put on Clexane to keep you safe, i.e. Clexane is used to take care that they suffer no hurt or damage.
The key to all this is a thing called Thrombocytopenia. This is the term used when your Platelet count is chronically low. Derek’s Platelet count sits between 105 and 120 (Normal Range is 150-400).
Like many things, Derek wanted to know more about Platelet Counts, warfarin, Sepsis and CAPS, so started looking at medical sites and looking at his blood results (we keep the all). In doing this we discovered that, apart from Antiphospholipid Syndrome, there is another reason for low Platelets. It can be an indicator of Disseminated Intravascular Coagulation (DIVC). When you have APS, and you suffer DIVC, it is considered CAPS.
One thing that does NOT cause low Platelet Counts is Sepsis.
Back to the medical records. This time, we went to the Hutt Valley DHB records of when Derek presented at Hospital the day after Biopsy.
Remember, CCDHB did NOT bridge Derek for his Biopsy.
In Derek’s HVDHB medical records for the admission on the day after his biopsy (he was still not on any form of anticoagulation) it clearly states “Bloods Sent”, which means they had drawn blood to do a blood workup. This is routine practice in ED for diagnosing when someone presents as ill, rather than an accident.
One of the most basic blood tests done is a Compete Blood Count (CBC). This includes your platelet count. It also shows if you are fighting an infection of any type. It won’t tell you WHAT is wrong, but will tell you if SOMETHING is wrong.
When you suffer Sepsis, your Platelet count increases (150-400 is normal). So you would expect to see a CBC Platelet count of over 300. With Derek you would at least expect to see him IN range if he had Sepsis. In Oct 2012, when the Infectious Disease Registrar was contacted, he tried to convince people Derek had Sepsis. His platelet count of 125 would indicate otherwise, and at the time, Derek was suffering CAPS. Inflammatory markers were up, but platelet count was down.
When looking at HVDHB’s notes What we found instead of the blood results was the next note on the HVDHB file for that day stating “Blood and Pro not sent to the lab”. We can only presume that by this time it was decided to transfer him to CCDHB and as they were passing his care to another DHB they didn’t need the Bloods processed, and so destroyed them.
Derek was put in a Patient Transfer Ambulance and taken to CCDHB (different District Health Board, so different process etc).
After reading that the bloods were not done at HVDHB we had a look at the CCDHB admission records. The only mention of Bloods in the CCDHB’s notes was “Follow up Hutt Bloods”. They never took any bloods of their own, ever.
They only took bloods for cultures. Because bloods for cultures are put in a special bottle, they cannot be used for a general CBC. There is also no indication in his file, that they ever followed up with Hutt because if they had, they would have seen that Hutt destroyed their bloods.
CCDHB simply did cultures. And what, you ask, did the cultures show? NOTHING.
Based on no evidence, and having failed to do a basic blood panel, there was an ASSUMPTION of Sepsis. Not a PRESUMPTION. To be a presumption, you must base your belief on the weight of the evidence available. As there was no evidence of sepsis, and no bloods taken, they erroneously presumed Sepsis.
When he was re-admitted a week later because he was still very ill, they assumed again, based on no evidence, and no positive cultures, that it was still sepsis, and threw higher dose antibiotics at him.
The better presumption based on weight of evidence being Cessation of Warfarin, NO Bridging, an Invasive Procedure, followed by starting of warfarin again with no cover of clexane, would be a Mild CAPS event.
We have now had 2 separate, independent Dr’s suggest the same thing. To prove, or disprove either theory, all they needed to do was a CBC. However, this was something that was never done. Therefore a diagnosis must be based on weight of evidence, which leads to CAPS.
Not only did CCDHB try to kill Derek during Surgery, but also during his Biopsy. This is not acceptable practice and clearly fails the Oath of “taking care that they suffer no hurt or damage”
It seems that the more we look into Derek’s medical care, the worse we realise his care has been.
Our goal at present is to make the medical profession be held accountable for their lack of care and concern. Ignorance is no excuse for almost killing Derek, not once, but TWICE.
