Stress and Avoiding a Crisis
As previous readers know, my husband has Primary Adrenal Insufficiency, I do not.
One of my pass-times is to do quilting, and on New Years Day 2023, I decided to try and complete a quilt I was making.
I was using an embroidery module to quilt around the edge of the quilt so the machine was running at a good speed, without my control.
Derek was just getting up.
Not thinking, I went to pull away, a loose thread on the quilt. The frame it was in, was moving towards me, so the thread was coming closer to me, and away from the needle. As I grabbed it, the hoop started going very quickly in the opposite direction. I had hold of the thread, so my hand went with it. As the needle landed in my thumb I realised what had happened. But before I could react and turn the machine off, the needle came down for a second, 3rd and 4th bite at my thumb. Each impact doing more damage.
I let out a very loud yell and Derek called back, “what’s happened, what can I do”. Knowing the mess my thumb was in (I had released it from the machine and was heading to the kitchen sink, I yelled back “Not you, BJ.” My adult son was up stairs and I knew he could help where Derek would just feel sick as the adrenaline tried to surge through his body.
BJ had a quick look to see if he could see a needle in my thumb as I knew the needle had broken off. It wasn’t there so he wrapped my thumb in sterile dressing, I put a tea towel around it, and BJ went up stairs to get dressed.
I was thankfully already dressed. I went into the bedroom where Derek had stayed, and told him what had happened, and that I needed to go to the Accident and Emergency (ED) room at the hospital.
I then asked him about his steroids. He had taken 10 mg on waking, but that was several hours earlier. He said he had taken 10mg HC when I told him BJ needed to help me as that was his indication that what ever was wrong, was bad. I told him to take another 10mg (20 in total) as that was the minimum he needed.
We got to ED and checked in. We were told we would need to see the Plastics team for this type of injury, but that it was good as their team was on today, so we wouldn’t have too long to wait.
As good as their word, we only waited an hour before we were called to a back room to be assessed. First things first I had an x-ray to see if the needle was stuck in there still.
Derek waited in the treatment room while I went for the Xray. It only took one shot to see the cluster of needle in my thumb. The technician then took a second one, from a different angle, where they could clearly see 4 pieces of broken needle. Thankfully Derek wasn’t there to see the image.
After 10 years of living with Derek and his AI I knew the signs of low cortisol. I went back into the treatment room and looked at him. I immediately told him he needed to take another 10mg as the 20mg he had taken was clearly not doing a enough.
A Practice Nurse came in and gave me what’s called a ring block (local anaesthetic all around my thumb to numb it). It took a long time to work, but once it had he had a poke around but couldn’t find the bits of needle.
“Sorry, I can’t reach them, you will have the wait for the surgeon to come and have a go.”
Within 30 minutes, a Plastic Surgeon came in and took us to a treatment room where she started working.
The whole time Derek was sat in a corner, barely holding on to “normal” function. 2 hours after the 10mg, he took another 10mg.
The surgeon finished her first go at finding all the needle (7 pieces in total) and got the call that she needed to go into surgery for a more serious case.
I was left to have another x-ray and see if she had got everything.
She hadn’t.
So we had to wait until she finished the more urgent surgery, which took 3 hours, not one, before she came back.
She then had to re-anesthetise my thumb and start digging again. She found 3 more tiny pieces and stitched me up.
Derek took another 5mg of hydrocortisone.
It got to 7pm which is his normal time for taking his nightly dose of 2.5mg, he took another 5mg.
Over the day he took a total of 60mg of steroids. This was 2.5 times his normal daily dose. This didn’t make him feel good, but it stopped him from feeling sick or going into crisis.
As we sat waiting during the day, we joked that I injured myself and went to ED, and he would stay the night. In fact, this is no joke. Had we not both had the knowledge of how his body reacted to stress, and the share bull headedness to ignore the naysayers that insist you contact your Endo before taking a stress dose, he would very clearly have ended up in hospital in Crisis. And on New Years Day, we would not have been able to call an Endo to get “permission” to stave off a crisis.
STRESS CAUSES CRISIS. It is a fact that most with AI know. But isn’t also something many Endos don’t seem to get.
I have never been one to ask the Endo if Derek should take extra cortisol. Since his last crisis in 2014 (the last time we listened to an Endo on dosing, and low cortisol symptoms) Derek has not had a crisis. Rather, he has had several illnesses that have made him very sick, or several stress events that Could have made him very sick, but we have managed his AI and left the other things to the medical profession. In doing this, he has not had a crisis since August 2014.
We are very strong advocates for knowing your body, knowing your low cortisol symptoms, and no, don’t over do steroids, but do take them when needed.
I see a lot of people who clearly need to updose, who are afraid to, and are told “call your endo”. It worries me that this is happening.
We were already starting to learn about his condition and his symptoms by 2014 but when we did call to ask should he updose for the symptoms he was having, he was told no, it wasn’t in the books as a symptom, therefore it wasn’t low cortisol. We now know that for Derek, what he experiences IS a symptom of very low cortisol, and we updose accordingly.
Stress CAN cause a crisis, even the stress of seeing a loved one injured.
And for those saying, well you should have left him at home. No. Derek agrees, he probably wouldn’t have had the brain function to take the extra cortisol without being told in the first few hours, and not knowing what was happening, my son would have gone home at some point to find him in Crisis. He was better off with me, where I could keep an eye on him.
The Dentist and the Dragon
The Dragon
As many of my readers know, we have a good medical system in New Zealand. It’s good, but it’s not great.
We also have a very different system when it comes to injuries and medical misadventures. For a start, in New Zealand we don’t call them Medical Misadventure. Oh, it’s an adventure. For some, like Derek, it’s the ride of your life.
But it is, like a broken leg, classed as an injury. For Derek, it’s a “Treatment” injury. He was injured because of medical treatment. But that’s history. Or should that be “His Story”.
When you suffer at the hands of the medical community, and are injured because of it, you get to have an assessment by the Government’s “Independent” “Insurance” Company.
Set up in the 1970’s, it was designed to stop any form of Litigation. Stop people having to pay crazy amounts of insurance just in case they suffer an injury. But like anything new, the concept and the reality can be vastly different.
This great independent organization, that was there for the injured, were under some very strict Insurance type rules. And like any good insurance company, they change the rules as often they change their pants. So, you have an injury you don’t know if you will be adequately covered.
When you read back through my blog you will see that Derek was covered for his Treatment Injury. This injury is his Adrenal Insufficiency. This impacts all parts of his life.
He had to give up driving because, although there is no obvious brain damage, he can no longer multi-task (Yes! I was lucky enough to marry a man that could multi-task). He is also one of the most intelligent men I have ever met. This is not me saying this, his School History (top 50 in the country) says this. He has been assessed as being unable to focus on more than one thing, his short-term memory is now not what it was, his ability to manage his stress is nothing compared to what it was.
But we manage. He still has his job. That’s thanks to an amazing boss.
So, the New Zealand insurance system, known as the Accident Compensation Corporation (ACC as we all know it) is our Dragon.
His treatment injury is permanent. It affects many aspects of his life, and if we need help because of that, we have to go into the dragon’s cave, and convince that dragon to stop breathing flames, and let us past, to get to the help we need.
To this end, he has a “Case Manager”. This is his direct contact in the dragon’s lair. But this Dragon is very hard on their workers. They are always being burned to the point the run, screaming from the lair, never to go back.
But on their way out, as the scream ENOUGH, they are supposed to contact all their “clients” and let them know they have reached boiling point, and they have run.
The Dentist
So why the back story?
Earlier this year Derek when for his normal checkup with the Dentist. She checked his teeth. They are ok. He needs more work the longer he is on steroids, but it could also be the fact he has “reached a certain age”. It comes to us all eventually.
She did x-rays, and then the bad news. “You need to have your 2 remaining wisdom teeth out.”
“OK can you do it?” Ah, the naivety of my darling husband. Hell NO! No way she will do it. She doesn’t mind the fact he is on warfarin to stop him clotting. He can even keep his INR within his designated range. She isn’t even worried that he has suffered CAPS. What she is terrified about is the stress it will cause him, and the very real, and high risk of an Adrenal Crisis.
“You need to see an orthodontist. They will do it under anesthetic, in hospital, where they can keep an eye on you, and monitor you properly.
Here’s where it gets a bit real. Oral and Maxillofacial Surgeons cost money. OK, not as much as in the US, but a lot for little old NZ. And I sure as hell am NOT paying.
I don’t mind paying $1500 to have it done in the local surgery, under local anesthetic. But an oral surgeon, anesthetist, a hospital bed for the day (or longer). No way. We would not have to pay that if he didn’t have AI, so no way am I paying.
Fighting the Dragon
Off to the Dragon’s Leir we go. Putting on our bravest face. Derek puts the words on paper, and I then writing them in a firm way.
Please Mr Dragon, can we have the money for the surgery. We should be covered as it’s due to the treatment injury he needs the high-risk extraction.
I don’t know if it’s the words I use, but we were told “Please, who would you like to assess you. We have Surgeons on our supplier list. Use one of them”.
Well, this is going to be a battle then. And the line has been drawn. We have to use one of THEIR suppliers. And anyone who has dealt with ACC know that their “authorized suppliers” are not there to spend ACC money, they are there to reduce that spend.
First blood to us. The Oral and Maxillofacial Surgeon we wanted to specifically use, is on THEIR list. We get our choice. But this is just stage one. The visit to the Orthodontist to get an assessment.
Does Derek need the extractions: Absolutely, and soon, there is already jaw damage being caused by the teeth. It will soon become painful, and there is a high risk of infection.
Does it need to be done by a specialist: Absolutely yes. These could be done in a standard dental surgery, but if something goes wrong, the teeth break or they are difficult extractions, then it would have to stop, and then it would become an emergency extraction.
Does Derek need General Anesthetic. Yes. Due to his complicated situation, a General, even though stressful on the body would be safer in case something goes wrong with the extraction.
We wait for the report to come back from the Oral and Maxillofacial Surgeon. It didn’t come. Oh, yes it did, it went to SPAM.
We then draft a very short email to Derek’s Case Manager and forward the report and the quote.
We decide that we will be willing to split the cost. We pay what it would cost in a normal dental surgery, ACC pay the rest. Now we wait to see what they decide.
Again, we waited. The first thing we were expecting was a letter from the Case Manager saying “thanks for your email, I will forward it for decision”. It never came. So, a week later we sent it again. Having fought battles with this Dragon before (and won) we did our usual.
“HI, you haven’t responded to our previous email. Please tell us what is happening, we are reattaching the documents in case they were stopped at your gateway.” We sent the email again 6 working days later. Then we sent one without the attachment. Still absolutely no response. So we had one more go. But this time we sent a copy to their “Complaints” department. We have learned through the 6 years so far of battling ACC, that we need to do this to make things happen.
We received a very quick response, but NOT from our case manager. The response included “ Ann has left ACC, this is why you wouldn’t have received a response yet. We have sent your email to someone else”. That was it. Still no idea who.
Apparently, “Ann” ran so fast out the door of the Dragon’s Leir, she didn’t have time to let anyone know she was going. We were put on to someone else.
We waited until “someone else” then responded to us.
So off to the complaints office we trot. This time it was a “Formal” complaint, not just a CC.
We want to know who our case manager is, why have we not had a decision on the dental work, why were we not told our case manager had left, oh, and why, after making the first “complain” was his right to have what is called “Driving for Independence” looked at, and why was our GP being asked whether Derek was now able to drive safely, and therefore cancel the driving provided.
Suddenly a swathe of emails from the Dragon’s Leir.
- SORRY! We have given you TWO case managers so this never happens again.
- SORRY! Please resend the information and we will get it to our assessment team urgently.
- SORRY! I hadn’t read the case file fully, and just saw that your driving was renewed 6 monthly, and that hadn’t happened so was reassessing your need. I now understand that it is a permanent (lifelong) Driving service we provide.
I guess, if you have to be given a sword to slay a dragon, it’s great when you get the RIGHT sword.
I have mentioned before, and if anyone fighting ACC reads this again, I will repeat. YOU HAVE RIGHTS! And for Derek, the key right is that they MUST take his injury into account whenever dealing with him. They had also failed to properly communicate with us, along with other violations.
For someone with a broken leg it’s easy. They simply say, here, have some crutches and come on in for an assessment. With a Mental disability due to an accident, it’s not as easy, and the sword they are given is NOT a strong one. They are disadvantaged as they must fight with all the might of someone fully functional, but who is missing two arms. And the sword can be taken at any time, just because they can.
But for Derek, they can’t do that. His covered condition is Adrenal Insufficiency (although the regularly get that wrong, and are currently calling it Adrenal Sufficiency). But as it is written everywhere that it is the lack of the stress response hormone, it’s a “Gotcha”. They are not allowed to cause him stress because it will make him sick, and that is not taking his injury into account.
And they have come to the party. Not quite with the best offer, but it’s a start, they have agreed to pay for the hospital, and the anesthesiologist. We haven’t finished, but we have time.
So now the preparation begins for the 24 January 2020 (baring anything going wrong in the meantime). Derek is scheduled for the first appointment of the day, in a private hospital, for his tooth extraction, and a day’s monitoring to ensure he doesn’t get sick.
Still a Single Road at Times
Aside
In 2013, my second post was very short. It was entitled “As single road at times”.
My posts back then were very short. They were a lot about how I was feeling, how we were learning to live with this condition strange new called Primary Adrenal Insufficiency (Addison’s Disease).
It was May 2013 that I began to Blog. In the last 6 years a lot of things have changed. But a lot have stayed the same, we have just learned to accept them and adjust to them.
Going to live performances, etc alone has become a new normal. I buy 2 tickets, and find someone to join me if Derek isn’t up to it. This could be a big show, or one that our children are performing in. Adjusting things so that we can go together has also become a “thing”. Whether that is by buying a matinée performance ticket instead of a night time one, or making sure he has a full day of rest, including a sleep, we will do what we need to, to keep going.
In May last year Derek had a set back. It was serious but it wasn’t obvious. A few blood tests went haywire for no obvious reason, he became a lot more tired than normal, and other subtle differences occurred. Despite this we carried on with life. We continued planning our big adventure overseas.
We did the trip. It was extremely tiring on Derek. We did a lot of walking with him using a walking stick constantly. We would walk, stop for coffee, walk, stop for a cold drink, walk, stop for a few photos, walk, stop for an ice cream (they make great ice cream in Europe). You get the picture.
Derek has been more tired than usual since getting home. It’s now 6 months since the trip and he is still a lot more tired than he was before May last year. So we have made more adjustments.
We have learned from that trip that you have to choose the fight. So now, if we are going out and we know it will be stressful, or very tiring on Derek, we use a wheelchair for him. After borrowing one for an evening we knew would be too hard on him without, he finally agreed that he really did need it. But not all the time, just for the harder events. It means that sometimes he can go out, and we can enjoy ourselves together. I still go out on my own because he is not up to it. Or we cancel our plans because I don’t want to go alone.
What we thought was just residual tired from the trip appears to not be that at all. After having more “crazy blood tests” we began to wonder. We have now looked at his bloods for the last 12 months, what ever is wrong, has been wrong since his various blood levels went haywire in April/May last year. But that’s ok, there is nothing we can do except keep an eye on his levels so that is what we do.
The reason we know things have not be right since May is that we keep track of all his blood tests. We don’t need to go the Doctor to ask, we can see. We know the symptoms, we know the signs and we can see his “normal” is changing and not for the better.
Having said that, in the words of a good friend who writes an amazing blog, he is clearly alive and will remain so.
Dehydration in Adrenal Crisis
When your sodium is normal, but you are dehydrated.
Dehydration does cause the serum creatinine to rise and the estimated glomerular filtration rate (eGFR) will, accordingly, fall. The degree of change is generally proportional to the degree of dehydration. Severe dehydration can actually cause acute kidney injury and may lead to a need for dialysis therapy.
National Kidney Foundation.
Water, water, every where,
And all the boards did shrink;
Water, water, every where,
Nor any drop to drink.
The Rime of the Ancient Mariner (text of 1834) Samuel-Taylor-Coleridge

Within the support groups there is always talk about dehydration being a sign of crisis, or impending crisis (or pre-crisis if that’s what you prefer to call it). To decide if you are in crisis, your electrolytes are checked. The standard sign is low sodium of <135 and/or high potassium of >5.2. The problem is when you don’t fit this criteria.
I hear many times, people believe they are in crisis, they feel horrible, they feel sick, they feel dehydrated, but when they present at ED they have their bloods taken, and are told they are “normal”, they aren’t dehydrated and therefore they can’t be in crisis.
What is being tested is sodium and potassium. I don’t often hear talk about creatinine.
Yet creatinine is the better teller of dehydration. Derek has had 3 crisis since diagnosis. The first two I didn’t get the blood test results for.
The 3rd one, because it was 18 months after diagnosis, I knew Derek’s normal blood levels. I was recording them on OneNote so I had them with me wherever I was, whenever bloods were taken. So I asked the Dr what Derek’s blood results were.
She insisted they were “all fine”. I kept pushing requesting very firmly that she told me the levels. She kept saying she couldn’t remember them, but they were fine. After pushing more and explaining that I knew what his normal was, so I would like to compare them, she finally told me that one was creatinine. She remembered this number because it was high, which meant his kidney function was low.
When I pointed out that it was changed and higher than his normal level she actually argued with me that it was better than the one she compared it to. I asked the date of that one. It was compared to when he was in hospital suffering CAPS and his worst and most life threatening Adrenal Crisis, before diagnosis. She wasn’t interested.
She was a Resident, which means she was learning how to be a Dr, she was a first year resident, so some basic knowledge should still have been in her brain.
Although at that time I knew Derek’s numbers, what I didn’t know was what those numbers meant.
After some more toing and froing we finally got Derek some SoluCortef, but still no fluid because his sodium had come back in the higher end of normal. I have since learned that his potassium was just above range and higher than normal for him.
The next day when the General Medical Consultant did ward rounds, his first comment was “So, pneumonia and adrenal crisis, and you are dehydrated.”
He had looked very quickly at a vein in Derek’s neck to confirm, but he was also looking at the blood results.
After I got home I started investigating what it was, when sodium was normal, that told him Derek was dehydrated, and why drinking water hadn’t helped.
Here’s what I found out.
Why Sodium and Water may not help. A very simple explanation.
Although Sodium can be a sign of dehydration, when you are on fludrocortisone sodium can be kept within range, but it won’t stop the kidneys from functioning below par.
When creatinine is higher, and therefore eGFR is lower than YOUR normal, it is a commonly known indicator of dehydration. The lower the eGFR number the more dehydrated you are.
But why don’t sodium and fluids help?
If you are really suffering low cortisol then that same low cortisol stops your body absorbing fluids so you not only need sodium, but you need cortisol, to keep you from becoming dehydrated. This is where Blood Pressure comes in. When you are first dehydrated, your body kicks in with a lot of other system mechanisms, to keep your blood volume up, hence you don’t suffer low BP immediately. It is the dehydration that determines when your blood pressure lowers.
The reason HC works to lower your BP is because it helps your body absorb the fluids it needs to increase blood volume, and thereby reduce the other mechanisms from activating, to try and balance things out. This won’t necessarily stop the crisis, but it will help you long enough to get more help.
So if you are told you can’t be dehydrated because your sodium isn’t low, ask what your creatinine (or eGFR) is. If they don’t know, ask them to find out. If they still argue, ask them what anti-diuretic hormone does, and the effect of that when you have low cortisol. It is one of a number of the mechanisms in your body to keep your blood volume up when dehydrated.
Generally, a high serum creatinine level means that your kidneys aren’t working well. Your creatinine level may temporarily increase if you’re dehydrated, have a low blood volume, eat a large amount of meat or take certain medications. – Mayo Clinic Website.
Back to Derek
When Derek is dehydrated he slips from Stage 2 to Stage 3 CKD. We have to monitor it regularly. IF you don’t know what your normal is perhaps you should find out when you are feeling healthy. This could save you a lot of medical issues when you are sick. And check out my post on “know your own normal” because sometimes, it too can save you.
One thing I remember is when Derek was in hospital in crisis before diagnosis, after 3 days they had to stop the fluids as his body was swelling up, and wasn’t absorbing the fluids. His kidney’s were failing, his blood pressure had started going down, and fluids were not working as he was just absorbing into tissue, his blood volume was going down.
A number of people have asked why they get fluids and fee better, before they are in crisis. these people still appear to have a very small amount of cortisol production. It may be that it’s enough to help absorb the fluids. Derek has no production, so at the time his body had nothing, including aldosterone, to help.
Preparedness is Key
I have a friend who also blogs about her Rare Condition. It’s well worth a read. I was “on line” with Sarah as we all went through these situations. It can be very stressful for someone who is lacking their natural stress hormones. But they are there for those who need help, any time of day or night.

Last night, I had to sit back and wait, helpless, while a fellow AI warrior slipped into adrenal crisis.
You see, I help moderate an online support group for people with adrenal insufficiency. Someone reached out to us for help, but we didn’t know where they were, how to reach them. Their online profile was locked down tightly, for security, and there was no way to know if this person survived the night.
**As I’m writing this, a friend of this person reached out to let me know that this person lived through the night… And I’ve burst into tears!**
On another group, a member frantically asked what they needed to do because they were afraid a crisis was imminent. They didn’t have a doctor to reach out to late at night, and didn’t know if their fear was warranted or not. They are new to this diagnosis.
Today, another…
View original post 304 more words
Chinese Whispers and Medical Research
Reminder, we are an AI patient and wife, not medical scientists, or medical Doctors. This is based on our own observations and experience even though we do discuss legitimate research here.
The origin of the term “Chinese Whispers” isn’t clear according to the wonderful Internet. It has also been called “Russian Scandal” or in the US “Telephone”. We all know what it is and have probably played it. You say a phrase or sentence, whispered into some’s ear. They then, without confirming what was said, repeat that phrase to the next person. This continues until everyone has heard the phrase once.
The challenge is to pass the message through a number of people without it becoming misheard and altered. The enjoyment of the game is that regardless how careful you are, the final message heard invariably is not what was originally said. It is used to show how gossip can affect outcomes, how we feel, what we believe, who we trust. The message being, if it isn’t from the horses mouth, then is it correct.
But were you aware that it can also happen with the written word. Someone writes something, a person looks at it, takes from it what THEY are looking for, and ignores something that although the author thought was relevant, the reader felt was of no significance.
A good recent example would be from a New Zealand Senior School Exam question.
The exam asked pupils to write an essay on the following question: “Julius Caesar once said, ‘Events of importance are the result of trivial causes’. With reference to the causes and consequences of a historical event you have studied this year, analyse the extent to which you agree or disagree with Caesar.”(Otago Daily Times)
The students sitting the exam had a serious issue with the word Trivial. Apparently many of them didn’t actually know what the word meant. I wasn’t so much concerned with the question (or the word Trivial) but with the quote itself. It is a 1980’s rewrite of the original and its context has slightly changed with its reinterpretation.
10 years ago, I would have taken what was written in research as correct, accurate and as it’s peer reviewed, good methodology. But in fact, it’s not always. In reading research for Adrenal Insufficiency, Derek and I have discovered this happens in referencing and “quoting” research as well.
But why is that important?
It doesn’t seem important at all, in fact some could say it’s trivial. But it is those trivial little re wordings’, the leaving out of part of a statement of the not reading the entire document and therefore missing an apparently trivial piece of information, that can have a big impact on how people are treated, and how their Dr’s will, or won’t listen to them.
One example we are looking at currently is dosing. What is better? Twice a day? Thrice a day? Four times a day? Maybe even five?
Derek is currently researching the origins of the belief that 15-25mg HC is all that is required. In doing this, we have come across a number of discussions around how many times a day to dose. What we have found is inconsistencies, misquotes, and lack of acknowledgement of some of the results from an original paper that is quoted.
The Original Paper:
Ekman, Bertil & Bachrach-Lindstrom, Margareta & Lindström, Torbjörn & Wahlberg, Jeanette & Blomgren, Johan & Arnqvist, Hans. (2012). A randomized, double-blind, crossover study comparing two- and four-dose hydrocortisone regimen with regard to quality of life, cortisol and ACTH profiles in patients with primary adrenal insufficiency. Clinical endocrinology. 77. 18-25. 10.1111/j.1365-2265.2012.04352.x.
https://www.ncbi.nlm.nih.gov/pubmed/22288685Results:
The four-dose regimen gave a higher serum cortisol before tablet intake in the morning (P = 0·027) and a higher 24-h cortisol (AUC) (P < 0·0001) compared with the two-dose period. In contrast, a lower median plasma ACTH in the morning before tablet intake (P = 0·003) and a lower 24-h ln (ACTH(AUC) ) were found during the four-dose period. The patients preferred the four-dose regimen (P = 0·03), and the HRQoL scores tended to be higher (high score indicates better HRQoL) for the four-dose period. In summary, a four-dose regimen gives increased availability of cortisol and an enhanced effect with a less elevated ACTH in the morning in comparison with a two-dose regimen but the effect on HRQoL remains inconclusive.
The final statement is rather subjective. The patients FELT it improved their QoL, but statistical analysis of the questionnaires could not support how the real life patients perceived it. Is that a fault in the questionnaire rather than the actual results?
Articles (peer reviewed and published) citing the above reference and “quoting” the conclusion:
Paper 1
Amir-Hossein Rahvar, Christian S. Haas, Sven Danneberg, and Birgit Harbeck, “Increased Cardiovascular Risk in Patients with Adrenal Insufficiency: A Short Review,” BioMed Research International, vol. 2017, Article ID 3691913, 5 pages, 2017. https://doi.org/10.1155/2017/3691913.
https://www.hindawi.com/journals/bmri/2017/3691913/
Quote
Nonetheless, all regimens used so far fail to exactly mirror the physiological circadian rhythm, thereby having a negative impact on the metabolic system. However, other approaches like using a four-dose regimen were not able to show significant changes in quality of life, body weight, blood pressure, or glucose levels compared to a two-dose regimen [15*,16].
This report focused on the results of a small group over 8 weeks with 2 different dosing regimes. What they didn’t mention was the significant variation + of the: Free urine cortisol nmol/24-h 2 doses (337 ± 173) vs 4 doses (330 ± 93). Although the mean was close, the variation was very wide and over time, could this have a higher impact on other health outcomes. Also the preference to four doses a day was significantly higher than twice a day dosing preference for quality of life. Without the full document, and the figures, we could believe the above statement in it’s entirety.
Paper 2
Stefan R. Bornstein Bruno Allolio Wiebke Arlt Andreas Barthel Andrew Don-Wauchope Gary D. Hammer Eystein S. Husebye Deborah P. Merke M. Hassan Murad Constantine A. Stratakis David J. Torpy. (2016). Diagnosis and Treatment of Primary Adrenal Insufficiency: An Endocrine Society Clinical Practice Guideline. The Journal of Clinical Endocrinology & Metabolism, Volume 101, Issue 2, 1 February 2016, Pages 364–389, https://doi.org/10.1210/jc.2015-1710
https://academic.oup.com/jcem/article/101/2/364/2810222
Quote
One double-blind, randomized, crossover study evaluating two-dose vs four-dose hydrocortisone treatments (98) concluded that cortisol pharmacokinetics were more physiological on the four-dose regimen; surprisingly, participating patients preferred this regimen.
The preference was a statistically valid conclusion, yet this group were surprised at the result.
They appear to have got the information right yet although the document notes that HRQoL scores tended to be higher indicating a better HRQoL with four doses a day they still only recommend 2-3 doses a day, with a rider that “high frequency regimes and size-based dosing may be beneficial in individual cases”. They do recommend 3-4 doses a day for children.
Derek and I use this paper a lot the good work in it. You just have to know if using it for your Dr, the parts to point highlight. If you are in the US and you see a lot of non US researchers listed don’t worry as NADF do approve and reproduce this document for use within America so it is valid there as well.
Paper 3
Jitske Tiemensma, Cornelie D Andela, Ad A Kaptein, Johannes A Romijn, Roos C van der Mast, Nienke R Biermasz, Alberto M Pereira. (2014). Psychological morbidity and impaired quality of life in patients with stable treatment for primary adrenal insufficiency: cross-sectional study and review of the literature
in European Journal of Endocrinology. https://doi.org/10.1530/EJE-14-0023
https://eje.bioscientifica.com/view/journals/eje/171/2/171.xml
Quote
QoL did not differ between patients on a four-dose regimen and patients on a two-dose regimen, but patients on a four-dose regimen tended to report better QoL .
This one has me a little confused. One sentence which states QoL did not differ, AND reported better QoL?
Paper 4
Frédéric Castinetti, Laurence Guignat, Claire Bouvattier, Dinane Samara-Boustani, Yves Reznik. (2017). Group 4: Replacement therapy for adrenal insufficiency. Annales d’Endocrinologie. 78. 525-534. 10.1016/j.ando.2017.10.007
https://www.em-consulte.com/en/article/1184799
Quote (invalid cite?)
Hydrocortisone must be delivered in 2 or 3 doses per day, the first and highest dose on waking and the last (in the case of a 3 dose regimen) 4 to 6 hours before going to bed. An international cohort study of 1245 patients with primary adrenal insufficiency (84%) or secondary adrenal insufficiency (16%) underlined that the majority of patients were on a 2 or 3 dose regimen (42% and 32%) while other regimens were less common (one dose, 10%, other regimens, 17%) [2]. Neither of the two most common therapeutic regimens were shown to be better, but the number of comparative studies is quite small [21, 32, 33]
One paper references the original research to justify 2 or 3 doses a day, yet the original document had no mention of 3 doses a day.
Paper 5
Forss M, Batcheller G, Skrtic S, Johannsson G. (2012). Current practice of glucocorticoid replacement therapy and patient-perceived health outcomes in adrenal insufficiency – a worldwide patient survey. BMC Endocrine Disorders 2012 12:8. https://doi.org/10.1186/1472-6823-12-8
https://bmcendocrdisord.biomedcentral.com/articles/10.1186/1472-6823-12-8
Quote
The results from this survey are in line with a recently published clinical study [24] which showed that a majority of the patients preferred the four-daily dosing regimen to twice daily when comparing equal doses of hydrocortisone given either twice daily or four times daily. The reasons reported were less fatigue, more alertness during the day, less headache and a feeling that the treatment effect was less varying during the day. The patients had complaints after the study that a four-dose regimen may be difficult to manage in the long run [24].
This final document quotes things correctly and picked up on the information buried within the report. It looks like they may have actually read the document properly.
My take on this.
If your Dr had only read the original document, he would have no problem if you wanted to move to 4 doses a day, especially when you aren’t increasing your dose, but spreading it out. It was also noted that on 4 doses a day, there was the potential to reduce your overall daily dose. Yet if they read some of the other more recent documents they would say there is no difference, so why change?
Chinese Whispers? Or just misinterpretation? This is just ONE example Derek and I have looked at. There are many more out there. And these changes in wording, or missing wording, can actually have an impact on a persons’ health and quality of life.
Next time a Dr tells you that “according to X research, Y is the case” ask them if that is the original research, or someone’s interpretation right or wrong, of that research. Then check that he has read the original research or just the abstract? The answer to the latter question will probably be no, because in a busy practice, Doctors don’t have time to read all the research. It is up to the well-educated/informed patient to politely assist them by highlighting the significant parts. That is, if the Doctor is happy to work as part of a team, with your best health outcomes in mind.
The Half-life of Facts
Aside
I was watching QI this morning. It’s a show where the facts are “Quite Interesting”, and generally obscure.
This morning the episode said something I was so intrigued with, that I rewound it to.
It stated that “At medical college, they usually teach that half of what medical students will learn, will be considered untrue in 10-20 years. This is termed the “half-life of facts”. That is to say that you know that half of the information will be untrue, you just don’t know which half.”
I found that to be Quite Interesting. Enough so that I decided to look the fact up, and see if there was any truth to it.
Samuel Arbesman, a mathematician at Harvard, titled his new book “The Half-life of Facts”. When talking to the Economist, he stated:
For example, in the area of medical science dealing with hepatitis and cirrhosis, two liver diseases, researchers actually measured how long it takes for half of the knowledge in these fields to be overturned. They gave a whole bunch of research papers from fifty years ago to a panel of experts and asked them which were still regarded as true and which had been refuted or no longer considered interesting. They plotted this on a graph. What they found is that there is a nice, smooth rate of decay; you can predict that every 45 years, half of this particular sort of knowledge gets outdated.”
But why am I citing an article in the Economist. Because you probably know a Dr that is still using that 50% of knowledge that is now outdated. Yet they treat you based on that knowledge.
According to Dr. Michael Gold from the Medical University of South Carolina; To paraphrase:
“The half-life of medical knowledge is seven years.”
If Dr’s are not keeping up to date, they may be treating you based on what is now outdated knowledge. We have found one such Dr in the guise of the Medical Advisor of one national Advocacy group
He trained 50 years ago. Based on the half-life of facts, if he finished his training in 1970, by 2010, almost 50% of what he learned is outdated. Some of that is “knowledge” is still stating as fact which is on the groups public webiste. When we recently questioned this knowledge (which we showed with research papers to be obsolete) we were told by the Advisor “I don’t care.” (words in writing).
This attitude by the “Medical Avisor” of a major Advocacy Group for a rare condition leads to several questions.
- Why is he holding the position? Is it just that it has some kudos?
- How does his obsolete knowledge help patients today to live a better life when other Doctor use that “knowledge” to treat the patient.
Knowledge is Power, but obsolete Knowledge is DANGEROUS!
Continuing education is key to good Doctoring. And that continuing education must include reading recent research on the conditions they are treating and accepting that just because it goes against what they have been taught, doesn’t mean it is wrong, or that the Dr researching and promoting the new information is doing it “for ulterior motives”.
Next time you speak to your Dr, ask him the date of the last Research Paper was that they read? If it is before 2000, then there is a better than even chance that half that knowledge is obsolete, or will be in the next couple of years. Ask them if they have heard the term Half-life Of Facts.
Some will agree, others will get upset because they will be reminded that they are not as up to date as they should be, and others will probably refute the statement, or get angry about it. Most likely the latter, are so well past their half-life with knowledge, that they should perhaps be ignored completely.
The Expert Patient
I am updating this post on “the Expert Patient” as there seems to be a lot of discussion around giving Medical Advice in Facebook Groups.
Facebook Groups that are there for support of fellow patients with the same chronic illness are actally a good thing. And those that are expert patients shouldn’t be afraid to share their expertise (or vast knowledge) of a condition. Despite some groups classifying your sharing of that knowledge as “Medical Advice”, it’s not, as long as you don’t claim it is.
The NIH National Library of Medicine now states:
“The concept of “expert patient” has been developed in the last two decades to define a patient who has a significant knowledge of his/her disease and treatment in addition to self-management skills. However, this concept has evolved over the last years, and these patients are now considered, not only to be more efficient in the management of their own condition and communicating effectively with health professionals, but to also act as educators for other patients and as resources for the last, provide feedback on care delivery, and be involved in the production and implementation of practice guidelines, as well as in the development and conduct of research initiatives.”
Tattersall RL. The expert patient: a new approach to chronic disease management for the twenty-first century. Clin Med (Lond). 2002 May-Jun;2(3):227-9. doi: 10.7861/clinmedicine.2-3-227. PMID: 12108472; PMCID: PMC4954037.
There is a move in many countries to encourage this type of patient, and it is also being encouraged now in many groups.
These people are not medical practitioners, and do not purports to be so, and therefore their opinions are not “Medical Opinions” but those of someone who does have extensive knowledge of the condition.
You will notice they also state what they say as suggestions, things to ask your Medical Specialist, or things to look at. I have seen these people “lead the horse to water” and suggest taking the information to their doctors. the fact the doctor then disagrees, does not mean the Expert Patient is wrong, it simply means they have probably read differing research to the Endo, who is so over worked, they don’t have time to read the latest research, which contradicts what they read 20 years ago.
As far back as 2002 an article was written for the British Medical Journal encouraging patients to become “Expert Patients”.
Clin Med (Lond). 2002 May-Jun;2(3):227-9.
The expert patient: a new approach to chronic disease management for the twenty-first century. Tattersall RL1. Author informationAbstract
The expert patient: a new approach to chronic disease management for the twenty-first century, produced by the Department of Health, recommends the introduction of ‘user-led self management’ for chronic diseases to all areas of the NHS by 2007. The premise is that many patients are expert in managing their disease, and this could be used to encourage others to become ‘key decision makers in the treatment process’. Furthermore, these expert patients could ‘contribute their skills and insights for the further improvement of services’. It is hypothesised that self-management programmes could reduce the severity of symptoms and improve confidence, resourcefulness and self-efficacy. It is stressed that this is more than just patient education to improve compliance. Instead there should be ‘a cultural change…so that user-led self management can be fully valued and understood by healthcare professionals’. I point out that these ideas, while welcome, are not particularly new. Achieving the desired culture change will not be easy.
“Expert patient”—dream or nightmare?
BMJ 2004; 328 doi: https://doi.org/10.1136/bmj.328.7442.723 (Published 25 March 2004)Cite this as: BMJ 2004;328:723:
The concept of a well informed patient is welcome, but a new name is needed
Since the chief medical officer for England first introduced the term expert patient, it has been picked up and used very widely.1 During this time, the notion of the expert patient seems to have been criticised by doctors at least as much as it has been welcomed.2 If one asks lawyers, architects, social workers, or management consultants whether they prefer clients who take an interest in the issues they face and are motivated to work in partnership to achieve successful results, the answer seems obvious. So why does the idea of expert patients provoke such antipathy within the medical profession?
There is even a Training Course across England called the “The Expert Patient Program which states:
“Creative thinking is key for the Expert Patients Programme (EPP), a thriving Community Interest Company that gives people more control over their conditions through cognitive therapy courses.
It has made a particular difference to people with long-term illnesses, such as diabetes, arthritis or respiratory problems, by teaching them how to self manage and monitor their own symptoms. “It’s giving patients more control,” says Renata Drinkwater, Chief Executive (interim). “Courses like these are proven to make a difference. They boost confidence and, in some cases, can delay the onset of other conditions. They also have other benefits, like reducing the amount of times the patient needs to go into hospital or use Accident and Emergency.”
Conclusions
So, will the vision set out by Professor Donaldson and the Expert Patient’s Task Force work? The simple answer is ‘no’, unless there is a sea change in attitudes among patients and, more importantly, healthcare professionals.
What About You?
As someone with a chronic illness, would you consider yourself an “Expert Patient”? Do you consider your Dr a Good Dr or a Bad Dr. Is he bad because he has a history of harming patients, or a bad Dr because he doesn’t know your specific condition.
As a patient with a chronic illness you go to your Dr expecting a good level of knowledge, and that they keep their knowledge up to date.
You go to a specialist with the same expectation.
What happens though if the chronic illness you have is rare condition? If your Dr or Specialist only has 1 patient with your condition, but over 1000 with a more common one. Do you expect them to keep their knowledge up to date?
The reality is, if you have a rare condition, you can’t and shouldn’t expect them to be as up to date as you want, or to have the knowledge you would like, at least not when you are a new patient. It’s different if you have had them for 2, 3, 4 or more years.
Instead, what you CAN expect, is to be listened to, to have them acknowledge that it is a learning process for you both, and that if you are able to provide relevant up to date information, they will accept it and not dismiss it because it wasn’t what they learned when they were training 20/30/40 years ago.
Yet this is also not always the case. So instead you learn what you can about your condition, to fill the gaps and hope you can at least work around your Dr.
In truth, a patient goes to the specialist wanting help to improve their quality of life. If you are lucky your specialist, knowing you are coming, has done a quick review of your medical notes, a quick read up of the condition. But with that, they have decided, almost before you walk in the door, what treatments they will or will not offer. If you ask a question they are not expecting, you take them off guard. But they don’t want to appear like they don’t know the answer (which they probably don’t) so they either ignore the question, or give some answer they drag from the back blocks of their brain where they remember something they heard once years ago, whether right or wrong.
These are the Dr’s we hear about in the forums. The ones that “don’t get it”. We get frequent cries of “I’ve fired my endo.” “My Dr is an Idiot.” “I can’t find a decent Dr who knows anything.” And I can see why they say it. I have heard the horror stories of medical appointments, ED/ER visits, lack of knowledge and but refusal to acknowledge it. These Dr’s need training in your condition, but they are not getting it. Why? Is it lack of time? Lack of interest? Or maybe they don’t know where to start?
What would happen if, instead of leaving frustrated, angry, and ready to fire them, you sat down and tried talking to them as equals?
What if you opened up the consultation with a different tact. If, instead of expecting them to know everything, or worse, you go in expecting to have a bad appointment with them knowing NOTHING, you went in knowing they didn’t know anything, but were open to learning.
What would happen if you opened up the conversation with something like “I am struggling with my conditions, and with the general lack of knowledge and research available. I don’t know how you Dr’s keep up to date when there are so many rare conditions out there. I need to get a better quality of life, perhaps we could learn and work together on how to better manage my health.”
What would your Dr say? You are not challenging their knowledge, but you are also not putting expectations on them to know it all. If they take that bit well, perhaps go on with “Do you have any recent research I could read, or a website where I could go to get good up to date research on my condition so I can learn more about how to help myself”.
The worst that could happen is they dismiss you out of hand and go back to their personal ideas. If this happens you have two options, you can get upset and leave the consultation frustrated then go on line to rant. Or you could ask them straight what their objection to having a knowledgeable patient is.
By now you have nothing to lose
if you have already decided to leave
and find a new Dr?
You might get a surprise. You MIGHT get a Dr that is willing to work and learn with you.
The Expert Patient may not only need to be an expert in their condition, but also in negotiation. A Win/Win negotiation is an art. It requires giving the Dr something they really need (which may be stroking their ego) but also getting what you need, which is a Dr willing to work with you.
Dr’s won’t learn, if they are not taught and quitting a Dr because he doesn’t already know simply means that the next patient will get what you have, a Dr that has neither the time or interest to learn. You never know, you might awaken in that Specialist or Dr, a new interest in your rare condition. Then he won’t be a Dr to run from, but a Dr to run TO.
Biologic Half-Life of Hydrocortisone. Why is this important?
As Derek lives with Adrenal Insufficiency, we started looking into his steroid doses to work out whether he was on the best dosing schedule possible for him.
In 2016 we had an Endo appointment and asked for a Day Curve to confirm his dosing was right. It was refused. So we asked for 1 random cortisol blood test. This was agreed to, more to keep us quiet than that the endocrinologist was actually looking for something. What we didn’t tell him was what WE were looking for.
We both believed that his dosing at 3 times a day was leaving him with low cortisol in the middle of the day. The only way to show this was to have a random cortisol taken right before his second dose of the day was due. His dosing at the time was:
6.00 am – 10mg / 12.00 noon – 7.5 mg / 4.00 pm – 5 mg
The problem with this dosing was that by 2.00 pm every day he was feeling like he wanted to sleep, and felt “blah”. Some days he was also showing clear signs of low cortisol.
We had seen tables that said that cortisol had a Half Life of 8-12 hours, but that didn’t make sense. We had also seen other tables that said 2 hours. That was a big difference. We needed to know what was going on for Derek.
1 Blood Test Tells It All
On the day we had set for the test Derek took his morning dose as usual at 6am. We then did the things we normally do on a weekend, very little. At 11.15 we went to the Lab for the blood draw. We wanted it as close to his second scheduled dose of the day as possible.
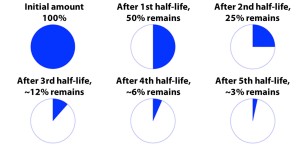
When we got the results it showed what we already believed. He was under range. Not just under range for that time of day, but below range completely. His cortisol was not lasting long enough in his body. But we had been shown tables that said it had a biologic half-life of 8-12 hours, so how could he be below range in 5.5 hours?
This didn’t make sense even though we knew it was right. So we started looking into what was meant by biologic half-life. What we found out is very scary, very concerning, and actually very dangerous.
What did we find?
BIOLOGIC HALF-LIFE CAN BE RUBBISH. It can be a false number, it shouldn’t be used in the way the below table indicates.
The table here is beening used by many groups/forums and on medical sites including on websites such as Endotxt.org, NCBI, and NADF so it must be right, surely.
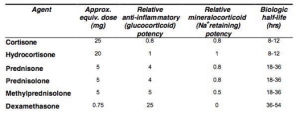
Do NOT use this to work out the half life of your Hydrocortisone or Prednisone for dosing!
Here it was, the table we got shown constantly. So Derek started looking further to try and find out where the biologic half-life came from. The first thing he found was the definition for biological half-life:
“Time required by a body to process and eliminate half the amount of a substance introduced into it. Also called biological half-life, biological half time, metabolic half-life, or metabolic half time.”
A number of variations of this table appear on the Internet and use the column heading Duration of Action. Other variations of this table simply classify the corticosteroids as short-, intermediate- or long-acting. The same numbers apply no matter what the column is referred to as.
If this column truly is a (biologic) half-life, and we apply the rule of 5 half-lives for complete elimination, then that would mean that Hydrocortisone would be visible in the body for up to roughly 2 days (40 hrs). Yet when Derek had a blood test before his morning dose, his cortisol was undetectable having had HC at 4pm the night before. That was 17 hours and no detectable cortisol. What would happen for the other 20+ hours? It was clear there was something seriously wrong with this table. None of this would be consistent with the title Duration of Action.
Also, if that was the case, you would only be prescribed cortisol once a day, not 3x, or more often now, 4x a day.
Where did this Table column come from?
There is no clear ownership of the table that we could find. It is used, copied, and the copy is referenced, but tracking back to the original hasn’t been possible by us. We do know it was created before 1980
He became very curious and decided to look further for the source of the information and came across this quote from “Principles of Endocrinology and Metabolism”,3rd edition, 2001, Chapter 78 “Corticosteroid Therapy” by Lloyd Axelrod.
This paper references the definition of:
“The commonly used glucocorticoids are classified as short-acting, intermediate-acting, and long-acting on the basis of the duration of the corticotropin (ACTH) suppression after a single dose, equivalent in anti-inflammatory activity to 50mg of prednisone.”
This is all about suppression of ACTH on high doses of prednisone, nothing to do with the amount of time you will remain within a safe cortisol range when you have Adrenal Insufficiency, yet Dr’s and patients alike use the table to justify twice a day dosing on HC.
So what are the implications of this table?
If someone uses this table to tell you that half-life is 8-12 hours for hydrocortisone they are wrong.
After looking for the original source of the table we discovered that the test was done as above, with a normal healthy person being given 50mg prednisone (approx 200mg HC). The only thing that can be taken from the original research is that 50mg prednisone will suppress ACTH production for a period of time. The hydrocortisone, and other drugs, were extrapolated from there (guess work based on poor knowledge).
If you had Primary Adrenal Insufficiency (Addison’s) and Hydrocortisone had a half-life of 8-12 hours, then taking HC every 6 hours would mean constant suppression of ACTH, and you would not have high ACTH after starting the steroid. But we know this isn’t correct because many with Addison’s still have some part of their Addison’s “Tan” due to raised ACTH. This is supported by the document below.
Professor Peter Hindmarsh is Professor of Peadiatric Endocrinology at University College London and Consultant in Peadiatric Endocrinology and Diabetes at University College London Hospitals and Great Ormond Street Hospital for Children. He is currently Divisional Clinical Director for Paediatrics at University College London Hospitals. He also runs a website called CAHISUS. He has written an article called GETTING CORTISOL REPLACEMENT OPTIMAL IN ADRENAL INSUFFICIENCY
The major goal of cortisol replacement in patients with adrenal insufficiency is to mimic as closely as possible, the normal pattern of cortisol production known as the circadian rhythm. The reason why we try to achieve this, is primarily to minimise side effects of over and under replacement and promote improved overall health. The two key factors are understanding the circadian profile and the pharmacology of hydrocortisone.
In this article Prof Hindmarsh talks about getting optimal dosing, and also looks at the absorption and clearance of people. What he showed is that there is a very large variation between people. The article is well worth a read. He also pointed out that the half life of hydrocortisone is a lot shorted than 8-12 hours, in fact, it is more like 70-90 minutes.
Another CAHISUS leaflet states this:
Hydrocortisone has a quick onset and the cortisol peaks to the highest level usually around 2 hours after being taken. The cortisol obtained from the tablet lasts in the blood circulation between 4-6 hours.
This is a change from an old document by Prof Hindmarsh which included the old figures as above. Things have changed, research has improved, and there is more knowledge out there.
What Does All This Mean in Steroid Dependant People?
For me? Gobbledygook. If you have a clear understanding of Half-Life, Clearance, and metabolism you may follow what is talked about in the studies. Personally, it confuses the heck out of me.
I do however, understand the concept of half-life. I first heard about it when watching a movie years ago about a child who had a certain amount of a chemical in his body at point C, and they claimed he had been given the chemical at point A. It was pointed out that he would have drunk a gallon of the chemical to have the amount still in his system because of the half-life of the chemical. The chemical had been very bitter and it would not be possible for the child to drink that much. I became very interested in half-life. I didn’t think then that it would be so important in Derek’s everyday life.
I had to ask Derek what everything he had found, and what the implications of half-life on hydrocortisone meant in layman’s terms, but even he struggled to explain it in a way that I could be easily understand. One thing he reminded me of is that while your Cortisol is going up, it is also being used.
I have also learned through this research is that even legitimate medical websites actually have misleading or wrong information.
When you are looking at a good way to dose for you, it must be an individual choice, based on how you feel between doses, whether you are willing to take multiple doses a day, and base it on signs and symptoms. The fact that Derek felt low at the scheduled time of his second dose of the day, and this was supported by a blood test that showed low cortisol, meant we could get the Endo to agree that dosing more frequently was the right option for him.
Now that he is on a better regime of 4 times a day, he functions a little better, he has a low base level of HC, and in the last 6 months, has lost weight without trying, but not in a bad way.
I wish you all luck with this as I understand that there are many Dr’s out there who are not interested in listening to their patients on more dosing throughout the day. One of the reasons for this is they don’t believe that you will be compliant, even though you are the one asking.
If they think you are asking for something that shouldn’t be done, then show them Prof Hindmarsh’s document above.
