I am a desk top publisher. I have used various desk top publishing tools from Aldus Pagemaker in the early 80’s to CS InDesign of the 2010 plus era.
I have created everything from A4 single page leaflets, to a 600 page, multi chapter Scientific document.
I understand more than some, how these larger documents are put together. When you have 2000 pages of information, written by 90 different contributors, across 5 different countries, and multiple regions and states within those countries this book must be constructed in a particular way.
So why is this important to my readers?
In my last blog, I briefly mentioned medical books can and will have out outdated study data when published.
In this blog post I am going to expand on that, and explain why we must all be aware of the implications of this.
When a large Cohort of people have input into a Text book on a particular topic, you will get differing opinions. When that book looks not just at a Broad topic, but then drills down into each sub-topic, it must be created by Section and Chapter.
Each Chapter is co-authored, then all chapters are put together at a publishing office to be produced in book form. This can, and does, lead to conflicting information in the book, if not carefully checked by someone who understands the different chapters.
In this case I am talking about Williams Textbook of Endocrinology.
Why this book in particular?
Williams Textbook of Endocrinology claims, in their own words:
“In this new edition we have strived to maintain Robert Williams’ original 1950 mandate to publish “a condensed and authoritative discussion of the management of clinical endocrinopathies based upon the application of fundamental information obtained from chemical and physiological investigation.”……..
With these goals in mind, we have once again assembled a team of outstanding authorities in the field who each contribute their unique expertise in the synthesis of current knowledge for each area.”
This is THE book that Endocrinologists go to for information.
But what happens when this book has failings?
Well, we in the Forums see the results of that every day.
I am only going to look at two chapters. I do not know the authors of these chapters, and I am not calling in to question their ability to read, and interpret their referenced material, or their knowledge of the Endocrine system.
What I am calling into question is the ability of such an important publication, to make sure that their information is up to date, accurate, and most importantly, consistent across chapters.
What led me here?
Quite simply, a comment from Derek.
We don’t go randomly into anything where his Adrenal Insufficiency, Antiphospholipid Syndrome, his Dysphagia, or any other conditions are concerned. We read, we research, we look at multiple published and peer reviewed studies on the subject.
In doing this, we have been able to stablise Derek’s condition and get him the best Quality of Life possible for him personally. This is not as good as some, but not as bad as others. This is because his limitations are different to everyone else. There are no two people with exactly the same concomitant conditions and therefore, there is no one size fits all solution to treatment.
We have found a number of things when it comes to Adrenal Insufficiency.
- A lot of “studies” are in fact people that have read other studies, and are giving their opinion on them by pulling them together and writing their interpretation.
- There is not a large amount of new information out there.
- Some of the new studies are looking at medical files, relying on Dr’s writing accurate notes (which many with AI have found to be inaccurate) and very few are actually talking to a large cohort of patients.
- Many tests on cortisol replacement are conducted on healthy subjects (or on a very small cohort (10-50) of AI sufferers, then applied to those with AI trying to mimic what happens in healthy people, not what happens in the chronically ill.
While researching something one night Derek found a snapshot of Chapter 15 from Williams Textbook of Endocrinology. He started reading it and found it so interesting that he was talking about getting hold of a copy of the whole book. It was over $200 NZ for an eCopy. Unfortunately, while reading it he came to the end of the available snapshot before he could finish what was being said.
He asked me if I had ever found reference to, or knew of this book. I hadn’t, so I started searching for it. I found the whole book, available for a limited time (the website would allow you to read it or X number of days), via an eBook. So I started looking up the information he was wanting.
What happened is that I found a different chapter to him, and found what I thought was the information he was searching for.
The problem with that was, the information I found, was different to what he was sure he had read. But how could that be. Surely, when talking about the same condition, the recommended treatment would be consistent across all chapters.
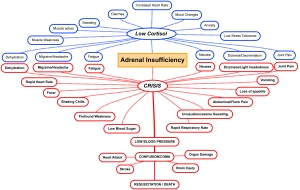
I am not talking about just the same subject, I am talking about the exact same condition of Adrenal Insufficiency, or your body being unable to produce it’s own Cortisol.
In this case, Long-Term Replacement Therapy vs Adrenal Steroid Replacement. They were different names, for the same information, that is Cortisol replacement for Adrenal Insufficiency (both primary and secondary).
OK you say, different names, nothing wrong there, the information will still be the same.
But it wasn’t! What I found, contridicted what Derek had found. But we were looking at the same edition of the same book, just different chapters.
There were two different theories on adequate timing and amount of replacement.
Here is where it affects those with AI
Most of those in the Forums, are taking either 2 or 3 doses of Hydrocortisone a day.
For many, this is what they were told when they started Hydrocortisone. Some of these people have been on the same dosing regime for over 50 years. It has never changed, it has never been considered they could change.
And this is still what they are being told. The amount and dosing schedule you are given, is dependant on the Dr that diagnoses you and his knowledge, or where he reads about the recommended dosing schedule.
Depending on which chapter the Dr reads the “Gold Standard” is either 2 doses a day or 3 doses a day. The amount will vary from 15mg/day as adequate, 20mg/day, and no more, or some are given a range from 15-25mg/day which they can work within.
The 1 consistency is that 30mg/day is considered too much for the average person with AI.
So where are these Dr’s getting their information, that it can vary so much.
Most likely it is all coming from the same book. But it will depend on which Chapter of Williams Textbook of Endocrinology the Dr is reading. And also, whether he is reading the text, or looking at the Tables.
Let me show you.
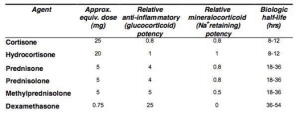
WILLIAMS TEXTBOOK OF ENDOCRINOLOGY, 13TH EDITION Copyright © 2016 by Elsevier, Inc.
CHAPTER 8 Pituitary Physiology and Diagnostic Evaluation
SECTION II Hypothalamus and Pituitary
Adrenal Steroid Replacement
Hydrocortisone is widely used for glucocorticoid replacement. The normal secretory rate of cortisol is 15 to 20 mg/ day, which is the recommended total daily dose. As plasma circulating half-life of cortisol is less than 2 hours, three times daily dosing of a total daily requirement of 10 to 20 mg (5-10 mg in the morning, 2.5-5 mg at noon, and 2.5-5 mg in the evening) is recommended.
Reference: Howlett TA. An assessment of optimal hydrocortisone replacement therapy. Clin Endocrinol (Oxf). 1997;46:263-268.
Where is the problem. It recommends 3 times a day replacement.
However……….
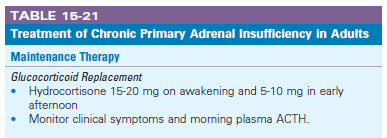
CHAPTER 15 The Adrenal Cortex
SECTION IV Adrenal Cortex and Endocrine Hypertension
The aim of long-term therapy is to give replacement doses of hydrocortisone to mimic the normal cortisol secretion rate (Table 15-21). ………
Reference: Howlett TA. An assessment of optimal hydrocortisone replacement therapy. Clin Endocrinol (Oxf). 1997;46:263-268.
Doses are usually given on awakening, with a smaller dose at 6 PM, but some patients feel better with three-times-a day dosing. In cases of primary adrenal failure, cortisol day curves with simultaneous ACTH measurements are advocated to provide some insight into the adequacy of replacement therapy.
Note the paragraph above a day curve is advocated. In the text book they then give a reference for this belief.
Reference: Arlt W, Rosenthal C, Hahner S, et al. Quality of glucocorticoid replacement in adrenal insufficiency: clinical assessment vs. timed serum cortisol measurements. Clin Endocrinol (Oxf). 2006;64:384-389.
CONCLUSIONS:
Our results suggest that serum cortisol day curves are of limited value in the monitoring of glucocorticoid replacement. Bone mineral density in AI is generally normal and does not require routine follow-up.
The conclusion of the Study referenced is that it is NOT required, yet the text book advocates it. Either the reference needs to be removed, or the advocating of the test should be reconsidered.
Then we have Table 15-21
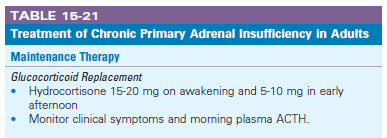
- HC Dosing of 15mg am and 10mg pm, or 20mg am, and 5mg pm to a max 25 mg HC per day
So you can see above, depending on where the Dr gets his information i.e., which chapter, depends on the dosing amount and schedule you are given.
One recommends 3 x day but only up to 20mg max, one says “2, but some feel better on 3”. The table (the easiest thing to look at when you are scanning 1800+ pages of information) states 2 x daily.
So Why the difference in Maintenance Treatment?
Simple, the articles are in two different chapters of the same book, but written or reviewed by 2 different groups, The first was by 1 person from Queensland and 1 from the States (Chapter 8) and the second by 2 people from England (Chapter 15). It is hard, but not impossible, to ensure the treatment is consistent, however, the distance, and disjointed way such a large publication is created can lead to different opinions and the inconsistencies.
If I was a Dr dealing with a patient with a Pituitary issue, I would possibly read SECTION II Hypothalamus and Pituitary; Adrenal Steroid Replacement.
Having read that, I would not then feel a need to go to SECTION IV Adrenal Cortex and Endocrine Hypertension; Long-Term Replacement Therapy to see that the replacement there was different. And if I did, what would I do? 2 or 3 doses a day? I certainly wouldn’t follow the references to read and make a decision for myself. I have 15 other patients to see that day. I will take the first answer I come across.
After all, this is the Expert Go To document to see what is needed. These specialists have already done the hard work. As the Dr, I have to read what I need to read.
But where does that leave the patient. Normally on a dose that doesn’t necessarily work for them, and in most cases, without any real cortisol cover for many hours of the day.
If you take a large dose in the morning, the half life is still the same, <2 hours. By the end of 4 hours, you are still having a dip.
The other problem is, much of the reference material is at least 15 years old, having been written in the 1990s. There is more recent research but instead of removing the old research, the just add to it, to increase the confusion for anyone who actually looks deeper into it.
And then there’s the Emergency Injection
Now a quick one about carrying your emergency shot. This same document, under Section IV; Adrenal Cortex and Endocrine Hypertension it very clearly states :
Parenteral preparations of hydrocortisone for self-administration may be required for patients living far from hospitals and those planning vacations.
Hence we have had death, and permanent impairment of patients who “live close to a hospital” who are being refused their emergency injection.
Many are refused their emergency injection based on that 1 paragraph, out of a book of 1900 pages.
Changes over the years.
After seeing all of this, I decided to see what had changed in the last 13 years, in the treatment of Adrenal Insufficiency. I have managed to access a copy of the 10th Edition, published in 2003. In comparing word for word, what is said about Long-Term Replacement Therapy there have been changes is wording, but not meaning, of a few paragraphs, and 4 paragraphs added near the end.
The changes in wording is of no importance as it didn’t change the context. However, in at least 13 years (I couldn’t get an earlier copy on line) these are the actual changes to treatment:
Added:
Progesterone is a mineralocorticoid antagonist, and the rising levels across pregnancy may necessitate an increased dose of fludrocortisone.
Added:
Patients should receive regular education regarding the requirements of stress-related glucocorticoid dose adjustment, which should involve the patient’s partner and family as well. Parenteral preparations of hydrocortisone for self-administration may be required for patients living far from hospitals and those planning vacations. (Italicised has not changed.)
Added:
However, patients with adrenal insufficiency on current steroid replacement regimens have significantly impaired health-related subjective health status irrespective of the origin of disease or concomitant disease.
Very last paragraph as if added as an after- thought as reference was published at the end of 2014
Added:
Delayed-release hydrocortisone preparations, such as Plenadren, that more closely replicate normal circadian cortisol concentrations, have recently been licensed and approved; early clinical trials show improved quality of life in both primary and central hypoadrenalism compared to conventional twice- or thrice-daily hydrocortisone administration.
Very little has changed, including the table stating twice daily dosing in the Adrenal Cortex section of the endocrine Text Book. That is 13 years and we know that one of those statements is wrong. ALL those suffering AI SHOULD BE GIVEN THE EMERGENCY INJECTION!
This is Critical to the survival of an Adrenal Insufficiency patient.
So where to from here?
A well worded letter to the people that wrote SECTION IV Adrenal Cortex and Endocrine Hypertension; Long-Term Replacement Therapy with a request that they urgently update their information, and issue everyone with that update, to ensure the safety of patients with Adrenal Insufficiency is paramount, and that assumptions of competence on the part of their over worked, time poor medical practitioners, is corrected to take into account a of lack of knowledge by the Endocrinologist who, never having had an AI patient before, just treat one.
Also Endocrinologists must be given consistent information no matter where in their Bible they look (or where on the Internet if needs must).